The most effective way to improve public health and to reduce healthcare costs (>50 %) is to educate the public about simple, cost-effective means to avoid activities that promote diseases and illness.
A related initiative is the need to inculcate a greater sense of personal accountability for one’s choices (indulgences) and downstream health outcomes.
Common factors that are responsible for disease, from a public health perspective, include
- Lack of social networks and community support systems, leading to feelings of isolation.
- Lack of access to healthy and nutritious foods that supply both macro- and micro-nutrients and eating processed foods, containing preservatives like nitrites, and endocrine disrupting chemicals (EDC) like phthalates.
- Lack of equity in public decision making processes, leading to exposures which damage health, usually among individuals with lower socioeconomic status, due to persistent environmental toxins in our air (e.g. volatile organic compounds, VOCs), and water (e.g., herbicide and pesticide residues).
- Lack of physical activity or exercise to promote relaxation, including daily stretching and deep diaphragmatic breathing (e.g., 20000+ year old practices like Qi Gong & Tai Chi Chuan, Yoga)
- Lack of restful sleep (~ 8 hours/day), which increases stress and system level inflammation and often leads to chronic diseases as sequelae.
I hope you find the content useful. Please feel to share your thoughts via the Contact page.
Be Well. Do Good.
******
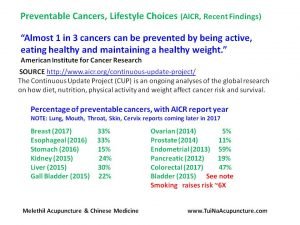
Preventing Cancer, Personal Choices
As the American Institute for Cancer Research (AICR) points out, we all have choices, which we must exercise, with regard to being accountable for our personal health. For example, being active daily affects our mental, physical, and social lives and provides a sense of fulfillment. Eating healthy foods and keeping an eye on our weight reminds us about the importance of regulating our metabolism and caring for our bodies, a lifelong commitment.
Interested in healthy recipes? Check out
http://www.aicr.org/healthyrecipes/?utm_source=mmenu
“Every dish has been rigorously tested and approved by AICR recipe developers, dietitians and staff. For a new AICR recipe every other week via email, sign up for our Health-e-Recipes.”
Preventing Cancer – A Personal & Public Health Option
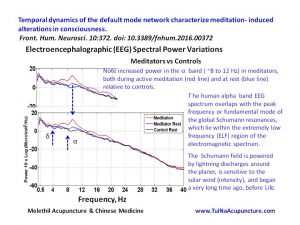
Meditation & Default Mode Network (DMN) Activation
During the last twenty years, fMRI research involving resting state networks of the brain, especially the DMN, has received a lot of attention. The DMN is a key brain network that underlies awareness of the “self within its environment” during periods of cognition not involved with a task orientation, e.g., resting, day dreaming. Functional changes in the DMN activity profiles have been linked to neurodegenerative pathologies like Parkinsonism, Alzheimer’s disease, and to normal physiological processes like aging.
Can meditation help improve attentional control and calm us down? Is the DMN one pathway by which we ‒ i.e., our cognitive processes, Mind ‒ can settle down from the unrelenting demands of our hectic lives?
This combined fMRI ‒ EEG research study offers insights into how meditation may rewire our brains’ functional connectivity patterns, without drugs.
excerpts (see article info below)
We have investigated dynamic alterations of the DMN using simultaneous EEG-fMRI, with the aim of characterizing the spatial and temporal changes caused by meditation induced alterations of consciousness. Using spatial ICA analysis of our fMRI data, we found that the posterior cingulate hub of the DMN was less strongly connected in meditators, which became further reduced during meditation. In contrast, the right middle frontal and left middle temporal gyri were more active in meditators and during meditation.
Meditation – Exploring Consciousness, Connections
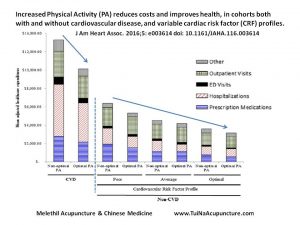
Physical Activity ‒ Improve Health & Reduce Healthcare Costs
This nice paper reminds us that increased physical activity (PA) can help us reduce both annual health care costs (~$2,500 per person, per year) and the risks of many chronic and resistant diseases, including those that affect our circulatory and respiratory systems. PA leads to better health outcomes and enhances the prevention of diseases like diabetes mellitus, cancer, hypertension, obesity, depression, and osteoporosis. In addition, it usually leaves us feeling better. The most critical factor in educating and implementing patterns of increasing physical activity, as a public health tool for use throughout our lives, is to allow for variations.
Variations in the duration, intensity, and frequency of physical activities allow for the expression of diversity among individuals. Asian techniques like Chi Kung (Qi Gong), Taijiquan, and Yoga offer adaptability in these 2000+ year old set of techniques to improve cognitive functions and general physical fitness ‒ agility (flexibility+ balance), cardiovascular capacity (endurance), and short term strength (power).
Keep moving.
What’s the Value of Exercise? $2,500. Link to NY Times article.
Increased Physical Activity & Cardiovascular Health Improvement, Reduced Healthcare Costs
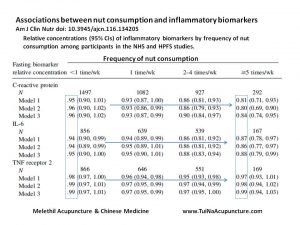
Go For Nuts, Any Nuts
Nuts as Dietary Interventions & Improved Inflammatory Biomarker Profiles
Booming Agers ‒ Sociological Perspectives
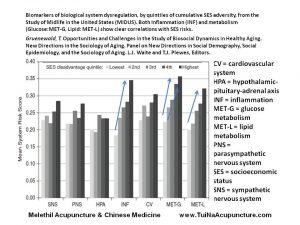
Humans are social animals but age deprives us of self-affirming and energetic connections with the people closest to us, due to both institutional and physiological factors. This book represents a structured study of the horizons of aging from sociological perspectives, both with regard to foundational issues like pre-analytic visioning (modeling) the matrix of interdependent factors and applied tools ‒ like clinical biomarkers‒ to test the models and their predictions.
Aging is a sequential process and proximate causes, i.e., developmental programming and life course, will affect long-term individual health outcomes.
From the book (see slides) below ‒
When individuals reach middle age, their health begins to change significantly and individuals diverge. This divergence is socially patterned, with more socially disadvantaged groups showing health declines much earlier than the more advantaged, including the onset of some age-related chronic conditions (e.g., hypertension) and disabilities. The greater divergence in health by groups appears to be due to “a long-term and cumulative process of health disadvantage over the life cycle”. Health in middle and older ages depends in part on social experiences during earlier stages.
A key theoretical and empirical question that could benefit from an institutional/life course approach to advance the study of aging is: Does growing older amplify or reduce existing disparities (by gender, socioeconomic position, race/ethnicity, and their intersections) in stressors, health risks, and material or emotional resources?
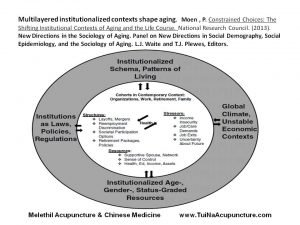
Aging in America, Socioeconomic Perspectives
The processes by which people are allocated to different roles, resources, and relationships and socialized to expect and choose different life paths depending on their age and gender (as well as their race and class) are the direct result of social policies as well as cultural conventions—norms and practices—related to them.
According to the author, a sociologist, institutions may be represented as conscious or unconscious rules about how to behave in, and think about, various social situations. To summarize, Institutions are not just places where organized social activities take place. Instead, they may be thought as “taken-for-granted schemas about ‘appropriate’ behavior—formal and informal rules and conventions representing collectively developed patterns of living which often reflect organizational and community answers to past problems and uncertainties.”
******
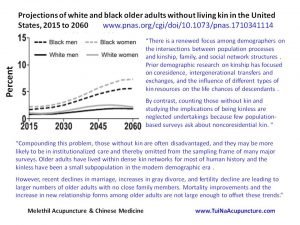
Looming Crises in Elder Care (United States)
As the authors note, in a related paper, “College-educated women and the least educated men have higher rates of kinless-ness. Kinless-ness should be of interest to policy makers because it is more common among those with social, economic, and health risks. It is more common among those who live alone, have little wealth, and are disabled.” The numbers of disabled are projected to increase significantly in the next few decades.
Elders in need of care are often dependent on family and friends to pick up when the healthcare system is unavailable to deliver. For example, the unpaid “informal” care provided by family and friends of Alzheimer’s patients matches the charges (~250 billion per year) billed to our healthcare system. What happens when this informal care network is no longer available? Governmentally sanctioned programs that lead to increased inequity, i.e., creating larger numbers of poor people, will add to the healthcare challenges we face.
For many decades, our healthcare systems have operated on the fantasy that providing drugs, with surgeries as a fall back option, represents the primary basis for improved public health. Lower cost options, including increased public education on the importance of nutrition based on whole foods and daily regimens of modest levels of physical activity have been neglected in our “formal” healthcare system. This situation has arisen apparently because medical doctors did not have these ideas presented to them during their initial training. Just as the nature of pain and of addiction to powerful prescribed psychotropic medications were also neglected. Unfortunately, our public sector funded healthcare programs, e.g., Medicaid, Medicare, continue to operate with these unsustainable perspectives.
The evidence to date suggests that educational programs offered at the community level, not in hospitals and clinics, and focused on the prevention of diseases offer the biggest return on investment of public (taxpayer) contributions. While these programs have to begin as early as possible in the life course of individuals to yield the best health outcomes, it is never too late to start along this path towards sustainable healthcare.
The persistent failure of government to acknowledge incompetence in healthcare delivery, both technical and administrative, represents a principal factor in the growing inequities that trouble this nation.